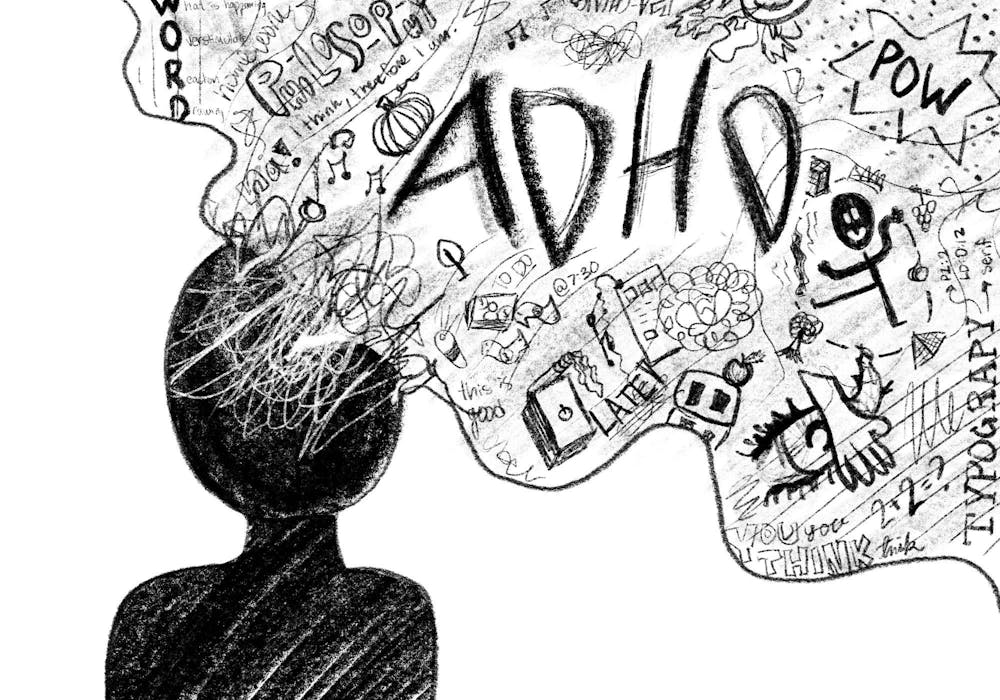
Overview
The neurodevelopmental disorder known as Attention Deficit Hyperactivity Disorder (ADHD) is typified by impulsivity, hyperactivity, and inattention. Although it affects people of all ages, childhood diagnoses are the most common. The field of treating ADHD has changed dramatically over the years, with drugs now being the mainstay for symptom management..
Notwithstanding,
the trajectory of ADHD medicine has been characterized by obstacles, disputes, and advancements. The future of ADHD treatment has been shaped by a revolution in ADHD medication in recent years due to advances in pharmacology, technology, and knowledge of the disorder. This article examines the history of ADHD medication, the condition of treatment now, and the exciting new discoveries that are fundamentally altering the way ADHD is treated.
The Development of ADHD Drugs
When stimulant medications like amphetamines were initially used to treat hyperactivity and inattention in the middle of the 20th century, that is when the history of ADHD medicine began. Methylphenidate, better known by its brand name Ritalin, was first used to treat ADHD in the 1960s. Some symptoms were reduced by these early drugs, but they also had serious adverse effects and raised questions about overprescription.
Pharmaceutical companies
Have improved the efficacy and safety of ADHD drugs over the years by creating novel formulations and delivery systems. In order to reduce drug peaks and troughs and offer more sustained symptom relief, extended-release formulations, such Adderall XR and Concerta, were developed. Alternatives to stimulants, such as atomoxetine (Strattera) and guanfacine (Intuniv), were also created for people with co-occurring disorders or those who could not take them.
Notwithstanding these developments, problems remained. A lot of people have negative effects like mood fluctuations, appetite loss, and insomnia. Furthermore, discussions and disputes among parents and the medical community have been sparked by worries about the long-term consequences of ADHD medication, notably on children’s growth and development.
Current Status of ADHD Drugs
For many people with the illness today, medication for ADHD is still the mainstay of treatment. Amphetamines and methylphenidate are two examples of stimulant drugs that are still often prescribed because they are good at easing the symptoms of ADHD. However, new formulations and delivery methods have been developed as a result of efforts to increase the safety and tolerability of these drugs.
The development of prodrug formulations,
Like lisdexamfetamine (Vyvanse), is one important breakthrough. Prodrugs are inert substances that the body metabolizes to create the active medication. In contrast to conventional amphetamine formulations, vyvanse, for instance, metabolizes into dextroamphetamine, which has a gentler onset of action and may lower the risk of misuse.
Apart from advancements in pharmacology,
Technology has also contributed significantly to improving the administration and tracking of ADHD drugs. People can monitor their symptoms, track their medication adherence, and improve communication with healthcare providers by using wearable technology and mobile apps. With the help of these tools, patients can actively manage their ADHD and get the most out of their treatment.
Furthermore,
a greater knowledge of how unique genetic variations can affect how an ADHD medicine works has been made possible by advances in genetic research. Pharmacogenetic testing, which examines a person’s genetic composition to forecast how they will react to particular drugs, has the potential to develop individualized treatment plans based on the individual biology of each patient.
Changing the Treatment of ADHD
The fields of neurology, pharmacology, and personalized medicine are about to witness a revolution in the treatment of ADHD drugs. The creation of tailored treatments that target particular neurological circuits connected to ADHD is one area of innovation. For instance, as ADHD is known to cause dysregulation of the dopamine and norepinephrine signaling neurotransmitter systems, researchers are looking for novel therapeutic targets in this area.
Furthermore,
Non-pharmacological therapies that might supplement or even replace conventional drug techniques have great potential in the field of neuromodulation. With the ability to modulate brain activity without the need for medication, techniques like transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS) are being researched as potential treatments for ADHD.
Furthermore, there is a great deal of promise for individualized and flexible interventions when digital therapeutics and artificial intelligence (AI) are combined with ADHD management. In order to predict individual responses to medication and enhance treatment tactics, artificial intelligence (AI) systems can evaluate large volumes of data, including genetic information, brain imaging scans, and real-time symptom monitoring.
In summary
With the advent of stimulant medications in the middle of the 20th century, the field of ADHD treatment has seen substantial change. Millions of people with ADHD now have hope thanks to safer, more effective medications that have been developed as a result of advances in pharmacology, technology, and our knowledge of the illness. Genetics and digital techniques will enable tailored, focused therapy that will shape the future of ADHD medication. By utilizing these advancements, we are influencing a future in which people with ADHD will be able to receive individualized care that will improve their quality of life and optimize their outcomes.